
LUTETHIM-177 PSMA: A Radiopharmaceutical That Increases the Chance of Prostate Cancer Cure
Today, for cancer cells in patients with stage 4 prostate cancer that have already masticated to other organs (such as lymph nodes further distant from the prostate, bones, or liver) which are resistant to hormone therapy, although the cancer at this stage cannot be completely cured, Lutetium-177 PSMA (Lu-177 labeled PSMA-targeted radioligand therapy) in combination with regular cancer treatment can slow down the cancer’s progression (imaged-based, progress-free survival) and prolong the overall survival.
What is Lutetium-177 PSMA?
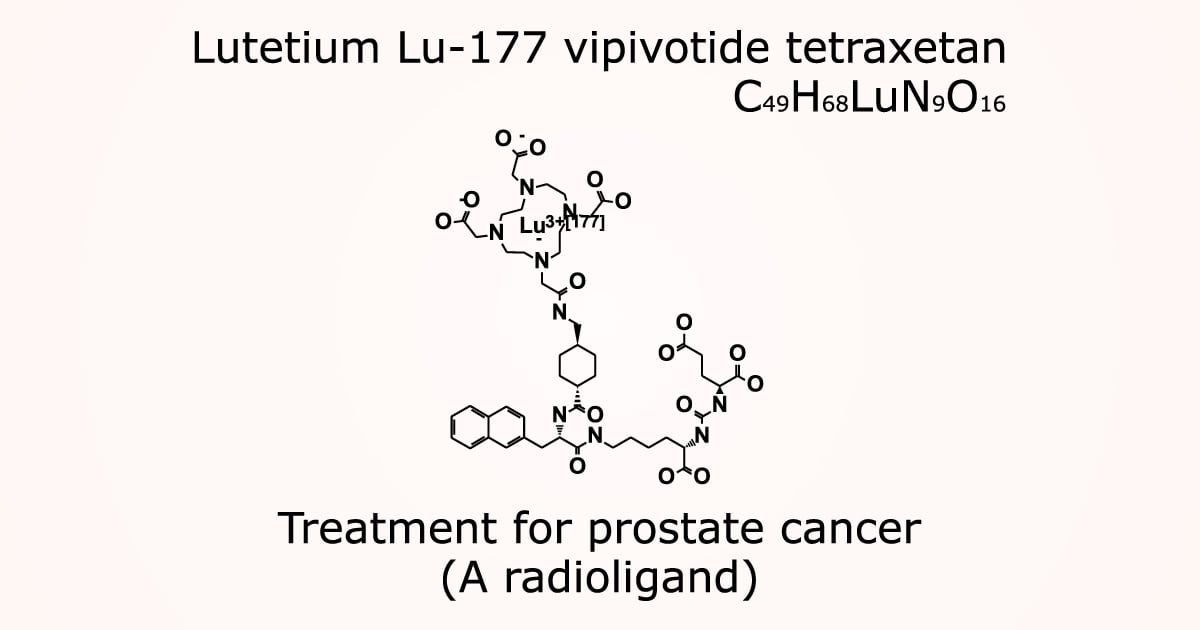
Lutetium-177 Prostate-Specific Membrane Antigen (Lu-177 PSMA) uses the Lu-177 radiation to destroy prostate cancer cells. Through beta-ray emission, Lu-177 molecules act as ligands and attach to the receptor PSMA on the cancer cells surface, yielding an image of the cancer; especially as PSMA generally reacts strongly to the radiation on the cancer cells of adenocarcinoma type – with a stronger reaction indicates a more severe cancer. Thus, the beta-ray radiation of Lu-177 PSMA will destroy cancer cells in the specific areas, reducing the size of the cancer and curtailing its spread. This enables a better biochemical response as well as clearer radio images, while also reducing the pain from the cancer in other organs along with, possibly, the PSA indicator. In addition, the toxicity of the radiation is low.
Indications and Considerations of Lutetium-177 PSMA Treatment
Currently, Lutetium-177 PSMA is not yet the primary treatment for prostate cancer patients whose cancer has already spread to other organs and become resistant to hormone therapy, as it has progressed further. It is neither intended for patients who have undergone chemotherapy nor non-chemotherapy. To qualify for Lutetium-177 PSMA, the patient must exhibit a significant level of PSMA on a PET/CT scan. In such a case, Lutetium-177 PSMA treatment is a viable option, as most patients’ conditions tend to improve, with longer cancer-free periods. In general, patients will be able to receive this treatment every six weeks, 4 – 6 times.
What Is the Process of Lutetium-177 PSMA Treatment?
Before a Lutetium-177 PSMA treatment can commence, a multidisciplinary team of cancer specialists will need to carefully evaluate the patient according to the treatment criteria. The patient will undergo a PET/CT scan (PSMA) to determine the progress of PSMA, as well as related blood tests to assess the patient’s suitability for the treatment. The next procedure includes an intravenous injection of Lutetium-177 PSMA and a two-hour observation for side effects. If there is no issue, the patient can go home and return to take a PET/CT scan the next day to determine the areas that Lutetium-177 PSMA has congregated. After the treatment, the patient must keep the doctor’s appointments on a regular basis, for physical examinations to see how the body responds to the treatment.
Side Effects of Lutetium-177 PSMA Treatment
After the treatment, some patients may experience these common side effects:
- Fatigue
- Nausea
- Vomiting
- Dry mouth
- Loss of appetite
- Reduced bone marrow production and function – e.g., being pale, low white blood cells count, or low hemoglobin.
Benefits of Lutetium-177 PSMA
In cases where Lutetium-177 PSMA is used to treat patients whose prostate cancer has masticated to other organs and is resistant to hormone therapy – and even after a chemotherapy – as the cancer has advanced, there are indications that the treatment is beneficial to the patients when they cannot undergo a chemotherapy with docetaxel. Studies show that people treated with Lu-177 PSMA possibly have a better quality of life and are more tolerant as well as responsive to this treatment than chemotherapy2-4.
Contraindications of Lutetium-177 PSMA Treatment
There is no absolute contraindication for this treatment, but there are some relative contraindications to consider where Lu-177 PSMA can be applied after the conditions are resolved. These include patients who are unable to urinate, have urinary tract obstruction or bone marrow suppression. Furthermore, patients who cannot be isolated and have comorbidities must be carefully evaluated on an individual basis. For patients with final stage of prostate cancer whose expected survival is no more than 3 months, Lutetium-177 PSMA treatment may not be suitable, but palliative care should be their priority instead.
The response to Lutetium-177 PSMA varies from patient to patient, and a cancer specialist will be the one who determines the treatment. Currently, some factors associated with poor responses have been found: for example, patients with comorbidities, high FDG uptake in PET/CT, a high PSA level or doubled over a short period of time, etc.
Doctor Specializes in Radioactive Drugs for Prostate Cancer Treatment
Asst. Prof. Dr. Usanee Techavijit, Nuclear Radiologist, Bangkok Cancer Wattanosoth
Hospital Specializes in Prostate Cancer Treatment
Bangkok Cancer Hospital Wattanosoth is well-equipped to treat prostate cancer with a multidisciplinary team of specialists, cutting-edge tools and technologies to help patients return to a high quality of life.
References:
- Kratochwil C, Fendler WP, Eiber M, et al. Joint EANM/SNMMI procedure guideline for the use of 177Lu-labeled PSMA-targeted radioligand-therapy (177Lu-PSMA-RLT). Eur J Nucl Med Mol Imaging.2023; 50:2830-45.
- Stapathy S, Mittal BR, Sood A, et al. Lu-177 PSMA-617 versus docetaxel in chemotherapy-naïve metastatic castration-resistant prostate cancer: A inferiority trial. Eur J Nucl Med Mol Imaging.2022;49(5):1754-64.
- Ahmadzadehfar H, Rahbar K, Baum RP, et al. Prior therapies as prognostic factors of overall survival in metastatic castration-resistant prostate cancer patients treated with (177Lu) Lu-PSAM-617 A WARMTH multicenter study (the 617. Trial). Eur J Nucl Med Mol Imaging.2021;48(1):113-22.
- Barber TW Singh A, Kulkarni HR, et al. Clinical outcomes of Lu-177 PSMA radioligand therapy in earlier and later phases of metastatic castration-resistant prostate cancer grouped by previous taxane chemotherapy. J Nucl Med. 2019;60(7):955-62.