
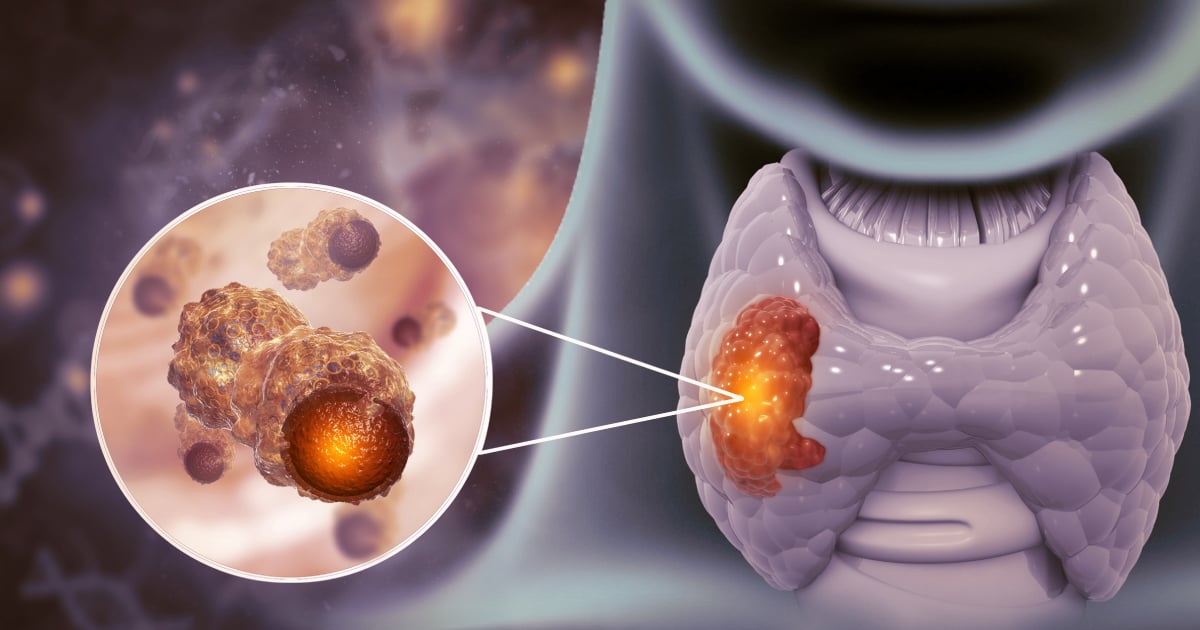
Knock Out Thyroid Cancer with I-131 Radiotherapy
Thyroid Cancer is more typical in women than men. Often, patients can identify the symptom when they discover a lump in their neck. Though the progression of thyroid cancer is generally well-defined, it can also spread to lymph nodes or other organs such as lungs and bones. The principal treatment is to remove the thyroid first, followed by radioiodine (I-131) therapy to completely eliminate any remaining cancer cell after the surgery.
Radioiodine, Iodine-131 Therapy
This medical treatment uses iodine-131 (I-131) which is a radioactive substance that decays by means of beta ray emission. It also radiates gamma ray that can be used to locate the cancer through nuclear medicine imaging equipment, as the radioiodine usually attaches to the differentiated thyroid cancer cells. In general, I-131 is administered in the form of a capsule that the patient can swallow.
I-131 therapy is an additional treatment to the operation. It normally commences at least 3-4 weeks after the surgery, but is not mandatory for all patients. The treatment is usually recommended for patients who are at high risk of a recurrence, and will be assessed by an experienced specialist. Further, the dosage will need to be determined by a nuclear radiologist as well.
Radioiodine therapy is an absolute contraindication for pregnant women or breastfeeding moms.
Preparation for Radioiodine (I-131) Therapy (1,2,3)
The preparation includes a low iodine diet and Thyroid Stimulated Hormone (THS or TSH Stimulation) therapy.
A low iodine diet means eating food that has less than 50 micrograms of iodine per day for 1-2 weeks before the treatment, to allow the thyroid and/or thyroid cancer cells to absorb I-131 better and increases the chance of a successful treatment. The patient should avoid high iodine food – such as seafood or any food with seafood or seaweed as ingredients (e.g., fish sauce) – as well as vitamins that contains iodine or food with iodine additive. It is safe, though, to consume salt that has not been iodized as salt deficiency can cause hyponatremia or low blood sodium level.
There are 2 main types of TSH stimulation in order to increase Thyroid Stimulated Hormone to more than 30 mU/L. These are:
- Stopping thyroid hormone therapy 3-6 weeks after the surgery, or delaying the therapy following the surgery.
- Administering Recombinant Human Thyrotropin (rhTSH) before I-131 therapy.
Complications from I-131 Therapy(3)
Common complications from radioiodine therapy can be categorized as Early Onset and Late Onset. The common early onset conditions include:
- Acute Radiation Sickness – such as nausea, vomiting, fatigue and headache.
- Radiation Thyroiditis. This is in the form of a swelling or pain around the front of the throat which can occur 10-20% of the time during the first 48 hours after the therapy.
- Lymphedema. If the cancer has spread to the brain, it can cause swelling and hemorrhage in the brain.
- Salivary Gland Inflammation. This will cause swelling under the ear or jaw on both rides.
- Distorted Taste Perception. The condition is only temporary.
The late onset complications include chronic salivary gland inflammation, dry mouth, sticky saliva, and premature menopause.
What to do after I-131 Therapy(4)
- During the first week after the treatment, patients should refrain from spreading radiation to people around them by staying at least 2 meters away from others or, if need be, spending as little time as possible in their presence. This also includes sleeping alone or keeping the beds 2 meters apart as well as avoiding crowded areas or anywhere that is not possible to maintain a distance.
- Be mindful of radioactive contamination from urine, sweat and saliva – for example, seated over the commode and flush twice afterwards, wash hands frequently, do not eat or drink from the same container with others, wash laundry separately.
- Use contraceptives for at least 6-12 months.
- Take thyroid hormone regularly as prescribed by the doctor and keep all follow-up appointments as scheduled.
Doctor Experienced in Using Radioiodine (I-131) for Thyroid Cancer Therapy
Asst. Prof. Dr. Usanee Techavijit, Nuclear Radiologists, Wattanosoth Cancer Hospital
Click here for self-appointment
Hospital Specialized in Radioiodine (I-131) Therapy
Wattanosoth Cancer Hospital is well-prepared to treat thyroid cancer with our team of experienced oncologists and multi-disciplinary doctors as well as modern medical equipment. We are ready to restore our patients’ quality of life.
References:
- Haugen B, Alexander E, Bible K, et al.2015 American thyroid associate management guideline for adult patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2016.26(1): 1-133.
- Avram A, Giovanella L, Greenspan B, et al. SNMMI procedure standard/EANM practice guideline for nuclear medicine evaluation and therapy of differentiated thyroid cancer: Abbreviated version. JNM.2022. 63(6):15N-35N.
- Luster M, Clarke S.E., Dietlein M, et al. Guidelines for radioiodine therapy of differentiated thyroid cancer. EJNMMI. 2008. 35:1941-1959.
- Dauer L.T., Hurley J. R, Brierley J. d. et al. radiation safety in the treatment of patients with thyroid disease by radioiodine I-131: practice recommendation of the American thyroid association.